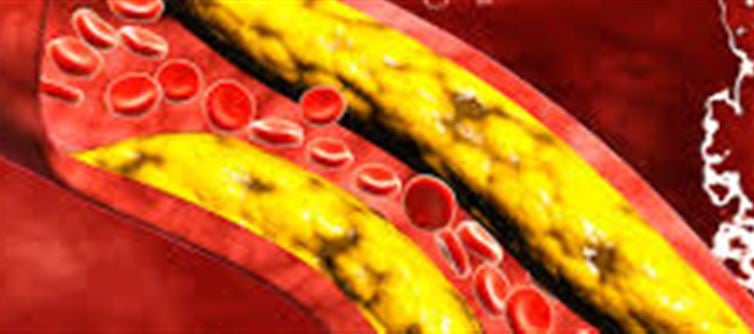
Pregnancy brings remarkable physical changes, many of which are completely natural adaptations to support the growing baby. Among these changes is a rise in cholesterol levels. While this increase is normal to some extent, significantly high cholesterol during pregnancy can raise important health considerations. Understanding why cholesterol rises, when it becomes risky, and how to manage it safely is essential for a healthy pregnancy.
Why cholesterol Levels Increase During Pregnancy
Cholesterol plays a vital role in fetal development. It helps build cell membranes, supports hormone production, and aids in the formation of vitamin D and digestive acids. Because of these demands, a pregnant woman’s body naturally ramps up cholesterol production.
Normal physiological changes include:
· Higher LDL (“bad”) cholesterol to support hormone production.
· Higher HDL (“good”) cholesterol to help transport fat where it’s needed.
· Increased triglycerides to provide energy stores for both mother and baby.
These shifts usually occur in the second and third trimesters. For most women, this temporary rise does not pose a problem.
When High cholesterol Becomes a Concern
Although cholesterol elevation is expected during pregnancy, excessively high levels can signal underlying issues or heighten certain risks.
Possible concerns include:
1. Pre-existing Hyperlipidemia
Women who already have high cholesterol before pregnancy may experience even more elevated levels.
2. Risk of Preeclampsia
Some studies suggest a link between very high cholesterol and increased risk of preeclampsia—a condition marked by high blood pressure and organ damage.
3. Gestational Diabetes
Elevated triglycerides may accompany insulin resistance, raising the risk of gestational diabetes.
4. Pancreatitis
Severely elevated triglycerides can trigger acute pancreatitis, a serious health emergency.
5. Long-Term heart Health
While temporary pregnancy-related increases are normal, extremely high levels may indicate an underlying genetic condition such as familial hypercholesterolemia (FH), which needs attention beyond pregnancy.
Symptoms: What to watch Out For
High cholesterol often shows no symptoms. However, signs of related complications may appear, such as:
· Persistent headaches
· Swelling in hands, feet, or face
· Upper abdominal pain
· Sudden weight gain
· Changes in vision
These symptoms require immediate medical evaluation.
Diagnosis: How cholesterol is Checked During Pregnancy
Cholesterol is usually measured through a simple blood test. Although routine lipid testing isn’t standard during prenatal care, your provider may monitor it if:
· You have a history of high cholesterol
· You are overweight
· You have diabetes or hypertension
· You have a family history of early heart disease or FH
Levels are often assessed during early pregnancy and again in the second or third trimester if needed.
Safe Management Strategies During Pregnancy
Managing cholesterol during pregnancy focuses on safe, non-medication approaches, unless medication is medically necessary.
1. Healthy Diet Modifications
A nutrient-rich diet can help control cholesterol levels without compromising fetal nutrition.
Tips:
· Choose whole grains, fruits, and vegetables.
· Opt for lean proteins: poultry, legumes, tofu, fish low in mercury.
· Include healthy fats like avocados, nuts, seeds, and olive oil.
· Reduce saturated fats (butter, red meat, full-fat dairy).
· Limit trans fats and ultra-processed foods.
2. Regular Physical Activity
Unless advised otherwise, moderate exercise is encouraged.
Safe options include:
· Walking
· Prenatal yoga
· Swimming
· Low-impact aerobics
Aim for 150 minutes per week, following your doctor’s guidance.
3. Weight Management
Gaining the recommended amount of weight—not too much and not too little—helps keep cholesterol within a healthy range. Your provider will guide you based on your pre-pregnancy BMI.
4. Medication Considerations
Most cholesterol-lowering medications, particularly statins, are not recommended during pregnancy because of potential risks to the fetus.
However, in rare cases—such as severe familial hypercholesterolemia—specialists may prescribe alternative treatments or closely monitor you.
Always consult your healthcare provider before taking or discontinuing any medication.
5. Managing Underlying Conditions
If high cholesterol is related to diabetes, hypertension, or thyroid disease, treating those conditions can naturally improve lipid levels.
Postpartum Cholesterol: What Happens After Delivery?
Cholesterol levels generally return to normal within a few weeks to months after childbirth. Your provider may recommend a follow-up lipid panel about 6–12 weeks postpartum.
Breastfeeding may help improve cholesterol and triglyceride levels—and benefits the baby, too.
If cholesterol remains high postpartum, your provider may discuss long-term management strategies, including medication options once breastfeeding considerations are addressed.
When to Seek Immediate Medical Care
Contact your healthcare provider right away if you experience:
· Severe or sudden headaches
· Vision changes
· Upper abdominal pain
· Shortness of breath
· Chest pain
· Swelling or rapid weight gain
These could indicate serious complications like preeclampsia or pancreatitis.
Conclusion
High cholesterol during pregnancy can be confusing and worrisome, but understanding the reasons behind it—and recognizing when it becomes a concern—helps ensure peace of mind and better health outcomes. For most women, the increase is temporary and harmless. Still, with proper monitoring, healthy lifestyle choices, and personalized medical care, high cholesterol can be effectively managed during pregnancy.
Disclaimer:
The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of any agency, organization, employer, or company. All information provided is for general informational purposes only. While every effort has been made to ensure accuracy, we make no representations or warranties of any kind, express or implied, about the completeness, reliability, or suitability of the information contained herein. Readers are advised to verify facts and seek professional advice where necessary. Any reliance placed on such information is strictly at the reader’s own risk.



 click and follow Indiaherald WhatsApp channel
click and follow Indiaherald WhatsApp channel